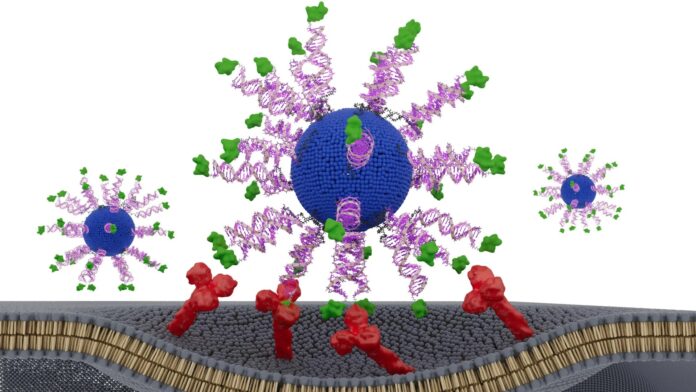
Researchers have discovered that a precisely engineered HPV vaccine dramatically enhances the immune system’s ability to destroy cancer cells, not by adding new components, but by rearranging existing ones at the nanoscale. The findings, published February 11 in Science Advances, demonstrate that even subtle structural adjustments can transform a weak immune response into a powerful anti-tumor effect. This breakthrough underscores the growing field of “structural nanomedicine,” pioneered by Northwestern University’s Chad A. Mirkin, where the arrangement of vaccine ingredients is just as critical as the ingredients themselves.
The Power of Arrangement: Beyond the “Blender Approach”
Traditional vaccine development relies on mixing antigens (tumor-derived molecules) with adjuvants (immune stimulants) – a method Mirkin describes as the “blender approach.” While effective, this method lacks precise control over how the immune system processes the vaccine. The new study flips this paradigm, showing that organizing these same ingredients into a meticulously designed nanoscale structure yields superior results.
The team constructed a spherical nucleic acid (SNA) vaccine – a globular DNA structure that penetrates immune cells – and systematically tested different configurations of its components. In humanized animal models of HPV-positive cancer and patient tumor samples, one configuration stood out: presenting an HPV-derived peptide on the surface of the SNA, anchored by its N-terminus, triggered up to eight times more interferon-gamma, a key anti-tumor signal. This configuration led to significantly stronger activation of CD8 “killer” T cells, the immune system’s most potent cancer fighters, and slowed tumor growth in mice.
Structural Nanomedicine: A New Era of Vaccine Design
This isn’t just about HPV. Mirkin’s lab has already applied this structural nanomedicine approach to vaccines targeting melanoma, breast cancer, colon cancer, prostate cancer, and Merkel cell carcinoma, with several candidates entering human clinical trials. The core principle is simple: structure matters. The same ingredients, when arranged correctly, can deliver stronger effects with lower toxicity.
“This effect did not come from adding new ingredients or increasing the dose,” said Dr. Jochen Lorch, co-leader of the study. “It came from presenting the same components in a smarter way. The immune system is sensitive to the geometry of molecules.”
Future Implications: AI and Repurposing Existing Candidates
Mirkin envisions using artificial intelligence to accelerate vaccine design, rapidly analyzing countless structural combinations to identify the most effective arrangements. This approach could also revitalize previous vaccine candidates that showed promise but fell short, simply by optimizing their nanoscale structure. The field is advancing rapidly, with over 1,000 commercial products already incorporating SNA technology.
“We may have passed up perfectly acceptable vaccine components simply because they were in the wrong configurations,” Mirkin stated. “We can go back to those and restructure and transform them into potent medicines.”
This research signifies a fundamental shift in how vaccines are developed, moving from brute-force mixing to precise nanoscale engineering. The implications extend beyond HPV, offering a powerful new tool in the fight against cancer and other diseases.